AN FDA-APPROVED BEVACIZUMAB BIOSIMILAR1
FLEXIBILITY DRIVES POSSIBILITY

Biocon Biologics is committed to being your flexible oncology partner. So you stay committed to providing targeted treatment opportunities.
Jobevne™ is highly similar to Avastin®, and is backed by an oncology biosimilars company you can trust.1,2

Demonstrated to be as safe and effective as Avastin1,2

Helps limit angiogenesis by inhibiting VEGF1

Designed to work with chemotherapy to prevent tumor growth3

Available for the Medicare Fee for Service (FFS) patient population
Jobevne™ is highly similar to Avastin®, and is backed by an oncology biosimilars company you can trust.1,2

Demonstrated to be as safe and effective as Avastin1,2

Helps limit angiogenesis by inhibiting VEGF1

Designed to work with chemotherapy to prevent tumor growth3

Available for the Medicare Fee for Service (FFS) patient population
SUPPORT
FOR YOU AND YOUR PRACTICE
From the moment you prescribe JOBEVNE, Biocon Biologics provides support to help start your Medicare FFS-eligible patients on therapy.
Coding and Billing
Information regarding applicable coding for JOBEVNE and its administration.
Prior Authorization/ Reauthorization Assistance
Requirement and submission details assistance, status tracking, and help with payer-specific forms.
BenefitS Investigation
Information on patient-specific insurance coverage requirements and patient cost-sharing aspects such as copay, coinsurance, and out-of-pocket maximum.
MY BIOCON BIOLOGICS™
Specialists are available to help Mon-Fri
8 AM-8 PM EST by calling 1-833-612-4626.
BIOSIMILARITY
YOU CAN COUNT ON
In a randomized, double-blind, Phase 3 trial, JOBEVNE demonstrated equivalent efficacy to Avastin in overall response rates of patients with stage IV non-squamous non-small cell lung cancer.3
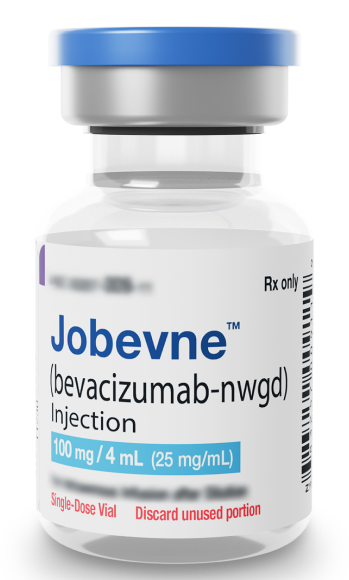
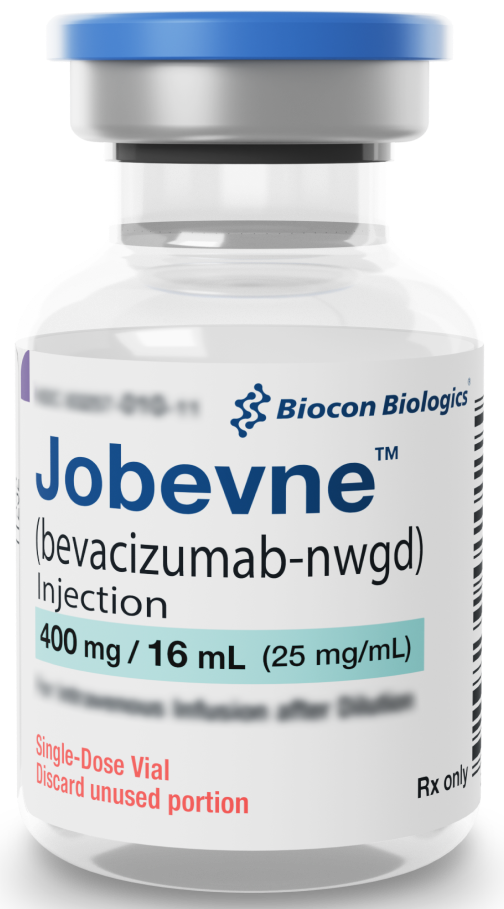
JOBEVNE IS AVAILABLE IN SINGLE-DOSE VIALS
The same familiar sizes you’ve been using with Avastin1,4
100 mg/4 mL single-dose vial NDC: 83257-009-11
400 mg/16 mL single-dose vial NDC: 83257-010-11
- Store JOBEVNE in the refrigerator at 36 to 46 °F (2 to 8 °C)
- Please see Full Prescribing Information for the dosing of JOBEVNE
Store FULPHILA syringes in the refrigerator at 36 to 46 °F (2 to 8 °C).
Please see Full Prescribing Information for the dosing of FULPHILA.

A FLEXIBLE ONCOLOGY
A FLEXIBLE ONCOLOGY
PARTNER

Biocon Biologics provides more than just biosimilars—let us flex our capabilities to meet your unique oncology needs.
With a portfolio of oncology biosimilars on the market and in our pipeline, we are committed to the long-term sustainability of biosimilars technology.
REFERENCES
INDICATION AND Important safety information
INDICATION
Fulphila® is indicated to decrease the incidence of infection, as manifested by febrile neutropenia, in patients with nonmyeloid malignancies receiving myelosuppressive anti-cancer drugs associated with a clinically significant incidence of febrile neutropenia.
Limitations of Use:
Fulphila is not indicated for the mobilization of peripheral blood progenitor cells for hematopoietic stem cell transplantation
IMPORTANT SAFETY INFORMATION
Do not administer Fulphila to patients with a history of serious allergic reactions, including anaphylaxis, to pegfilgrastim or filgrastim.
Acute respiratory distress syndrome (ARDS) can occur in patients receiving pegfilgrastim products. Evaluate patients who develop fever and lung infiltrates or respiratory distress after receiving Fulphila for ARDS. Discontinue Fulphila in patients with ARDS.
Serious allergic reactions, including anaphylaxis, can occur in patients receiving pegfilgrastim products. The majority of reported events occurred upon initial exposure and can recur within days after discontinuation of initial anti-allergic treatment. Permanently discontinue Fulphila in patients with serious allergic reactions to any pegfilgrastim or filgrastim products.
Severe and sometimes fatal sickle cell crises can occur in patients with sickle cell disorders receiving pegfilgrastim products. Discontinue if sickle cell crisis occurs.
Glomerulonephritis has been reported in patients receiving pegfilgrastim products. The diagnoses were based upon azotemia, hematuria (microscopic and macroscopic), proteinuria, and renal biopsy. Generally, events of glomerulonephritis resolved after withdrawal of pegfilgrastim products. If glomerulonephritis is suspected, evaluate for cause. If causality is likely, consider dose-reduction or interruption of Fulphila.
Thrombocytopenia has been reported in patients receiving pegfilgrastim. Monitor platelet counts.
Capillary leak syndrome has been reported after granulocyte colony-stimulating factor (G-CSF) administration, including pegfilgrastim products, and is characterized by hypotension, hypoalbuminemia, edema, and hemoconcentration. Episodes vary in frequency, severity and may be life-threatening if treatment is delayed. Patients who develop symptoms of capillary leak syndrome should be closely monitored and receive standard symptomatic treatment, which may include a need for intensive care.
The G-CSF receptor, through which pegfilgrastim and filgrastim products act, has been found on tumor cell lines. The possibility that pegfilgrastim products act as a growth factor for any tumor type, including myeloid malignancies and myelodysplasia, diseases for which pegfilgrastim products are not approved, cannot be excluded.
Myelodysplastic Syndrome (MDS) and Acute Myeloid Leukemia (AML) have been associated with the use of pegfilgrastim in conjunction with chemotherapy and/or radiotherapy in patients with breast and lung cancer. Monitor patients for signs and symptoms of MDS/AML in these settings.
Aortitis has been reported in patients receiving pegfilgrastim products. It may occur as early as the first week after start of therapy. Manifestations may include generalized signs and symptoms such as fever, abdominal pain, malaise, back pain, and increased inflammatory markers (e.g., c-reactive protein and white blood cell count). Consider aortitis in patients who develop these signs and symptoms without known etiology and discontinue Fulphila if aortitis is suspected.
Increased hematopoietic activity of the bone marrow in response to growth factor therapy has been associated with transient positive bone imaging changes. This should be considered when interpreting bone imaging results.
The most common adverse reactions (≥ 5% difference in incidence) in placebo-controlled clinical trials are bone pain and pain in extremity.
You may report side effects to the FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Please see Full Prescribing Information.
Copay Assistance
Access to FULPHILA for commercially insured patients with copay as low as $0.* See full terms and conditions.
BenefitS Investigation
Information on patient-specific insurance coverage requirements and patient cost-sharing aspects such as copay, coinsurance, and out-of-pocket maximum.
Coverage/Claim Appeal Assistance
Appeal requirement verification and appeal status/resolution tracking.
Coding and Billing
Information regarding applicable coding for FULPHILA and its administration (FULPHILA has been assigned a product billing code of Q5108).
Download the Coding and Billing Guide. ![]()
*Eligibility requirements apply.
Prior Authorization/ Reauthorization Assistance
Requirement and submission details assistance, status tracking, and help with payer-specific forms.
INSURANCE AND ALTERNATE COVERAGE
Patient insurance plan enrollment verification and identification of state programs, third-party charitable foundations, or other coverage options.
PATIENT BROCHURE
An informative guide for patients new to FULPHILA.
Download the Patient Brochure. ![]()
Download the Patient Brochure. ![]()
